Posterior Cervical Foraminotomy

Posterior cervical foraminotomy is a surgical procedure performed to relieve pressure on nerve roots in the cervical spine by enlarging the neural foramen—the passageway through which nerve roots exit the spinal canal. This procedure is often used to treat conditions such as foraminal stenosis, herniated discs, or bone spurs that may be compressing the nerve roots. Here is an overview of the posterior cervical foraminotomy procedure for patients:
Overview of Posterior Cervical Foraminotomy:
Indications:
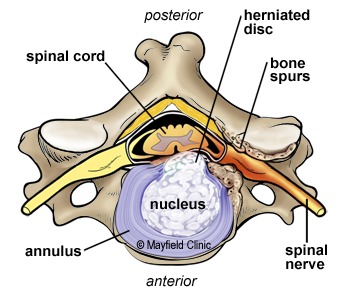
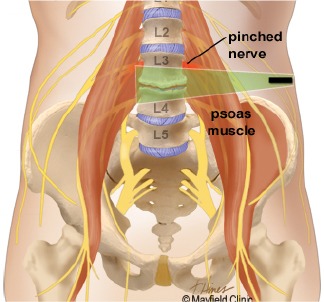
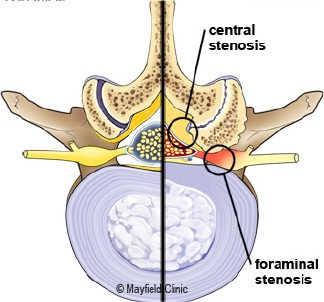
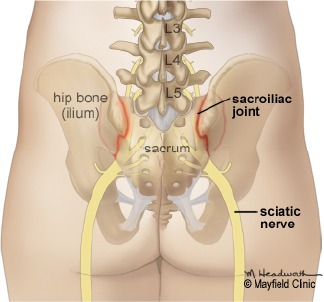
Foraminal Stenosis: Narrowing of the neural foramen, causing compression of the nerve roots.
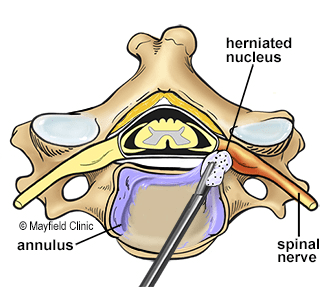
Herniated Discs: When a disc in the cervical spine herniates, pressing on nerve roots.
Bone Spurs: Abnormal bone growth that may encroach upon the neural foramen.
Preparation:
Medical Evaluation: Patients undergo a thorough medical evaluation, including imaging studies (MRI, CT scans) to assess the extent of the cervical spine issue.
Discussion with Surgeon: The surgeon explains the procedure, discusses potential risks and benefits, and answers any questions the patient may have.
Procedure:
Positioning: The patient is positioned face down on the operating table.
Anesthesia: General anesthesia is administered to ensure the patient is asleep and pain-free during the procedure.
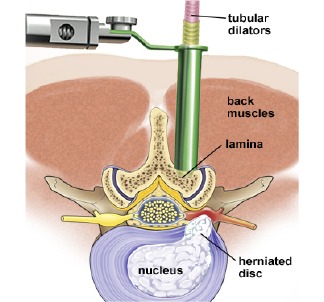
Incision: An incision is made in the back of the neck (posterior approach) to access the cervical spine.
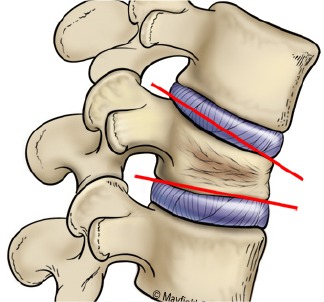
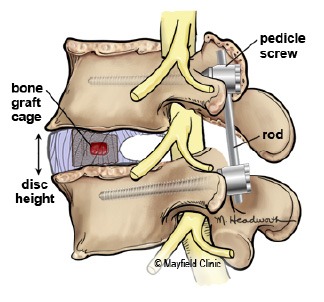
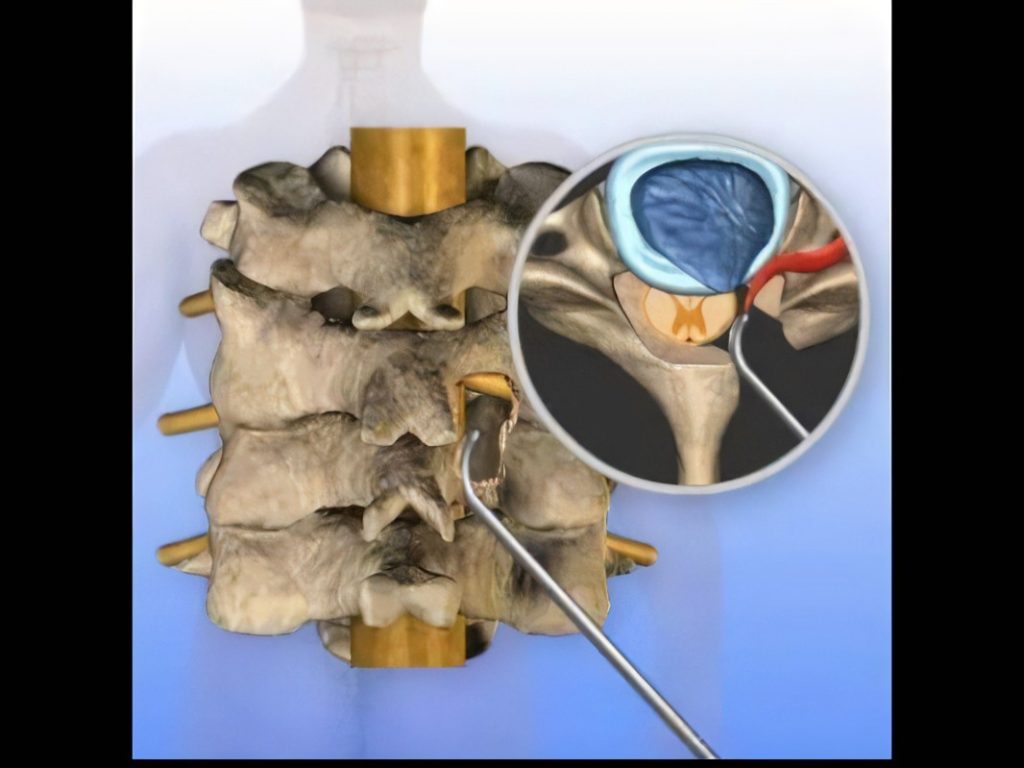
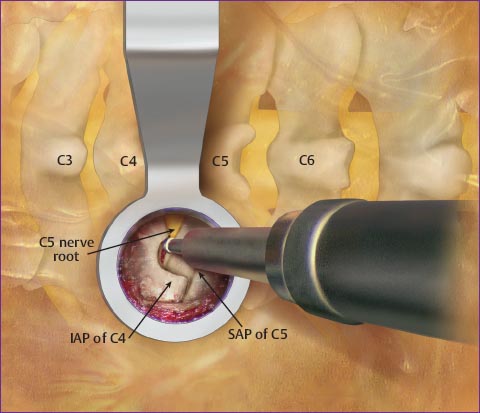
Laminotomy: Part of the lamina (the bony arch of the vertebra) is partially removed, exposing the neural foramen.
Foraminotomy: The surgeon uses specialized tools to carefully remove or trim parts of the bone or tissue that are causing compression of the nerve roots.
Decompression: The goal is to create more space within the neural foramen, relieving pressure on the nerve roots.
Closure: The incision is closed with sutures or staples.
Recovery:
Hospital Stay: The length of the hospital stay is typically short, often just one night.
Neck Brace: A neck brace or collar may be worn for a specified period to support the neck during the initial healing phase.
Physical Therapy: Rehabilitation exercises and physical therapy are gradually introduced to help restore neck strength and mobility.
Activity Restrictions: Patients are typically advised to avoid certain activities, such as heavy lifting or strenuous exercise, during the initial recovery period.
Follow-up:
Postoperative Visits: Patients have follow-up visits with the surgeon to monitor the healing process, address any concerns, and assess the effectiveness of the procedure.
Potential Risks and Considerations:
As with any surgical procedure, there are risks, including infection, bleeding, and complications related to anesthesia.
Nerve injury is a potential risk, although the procedure is designed to minimize this risk.
The success of the procedure in relieving symptoms varies among individuals.