Cervical Disc Replacement


Cervical disc replacement is a surgical procedure performed to address cervical disc herniation or degenerative disc disease in the neck. The procedure involves removing a damaged or degenerated cervical disc and replacing it with an artificial disc implant. The goal is to maintain motion at the affected spinal segment while alleviating symptoms such as neck and arm pain. Here is an overview of cervical disc replacement for patients:
Indications:
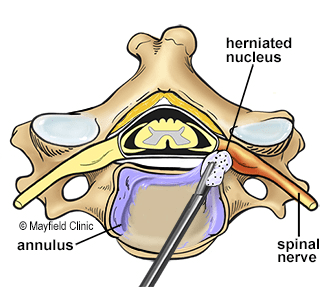
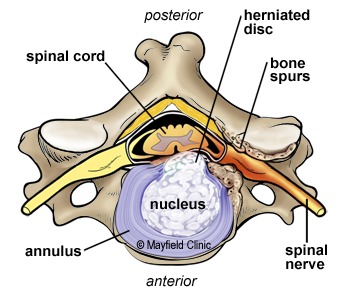
Cervical Disc Herniation: Protrusion of disc material that may compress nerves or the spinal cord.
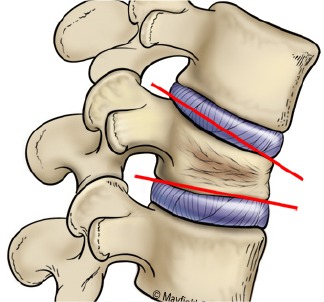
Degenerative Disc Disease: Wear and tear on the cervical discs, causing pain and reduced mobility.
Radicular Arm Pain: Pain radiating down the arm due to nerve compression.
Preparation:
Medical Evaluation: Patients undergo a thorough medical evaluation, including imaging studies (MRI, CT scans) to assess the extent of the cervical spine issue.
Discussion with Surgeon: The surgeon explains the procedure, discusses potential risks and benefits, and answers any questions the patient may have.
Procedure:
Positioning: The patient is typically positioned face up on the operating table.
Anesthesia: General anesthesia is administered to ensure the patient is asleep and pain-free during the procedure.
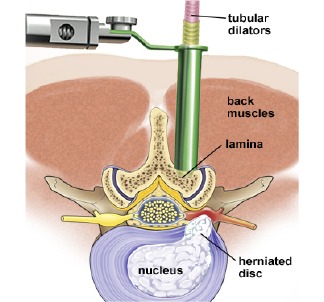
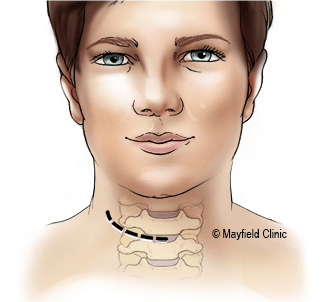
Incision: An incision is made in the front of the neck (anterior approach) to access the cervical spine.
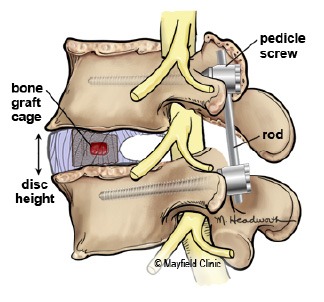
Discectomy: The damaged disc is removed, and any impinging material causing compression is cleared.
Artificial Disc Placement: An artificial disc implant is inserted to replace the removed disc. The implant is designed to allow controlled motion at the spinal segment.
Closure: The incision is closed with sutures or staples.
Recovery:
Hospital Stay: The length of the hospital stay is typically one to two days.
Neck Brace: In some cases, a neck brace or collar may be worn for a specified period to support the neck during the initial healing phase.
Physical Therapy: Rehabilitation exercises and physical therapy are introduced gradually to help restore neck strength and mobility.
Activity Restrictions: Patients are typically advised to avoid certain activities, such as heavy lifting or strenuous exercise, during the initial recovery period.
Follow-up:
Postoperative Visits: Patients have follow-up visits with the surgeon to monitor the healing process, assess the effectiveness of the procedure, and address any concerns.
Imaging Studies: X-rays or other imaging studies may be conducted to evaluate the placement and function of the artificial disc.
Potential Risks and Considerations:
As with any surgical procedure, there are risks, including infection, bleeding, and complications related to anesthesia.
Artificial disc replacement may not be suitable for all patients, and the choice of procedure depends on individual factors.
The success of the procedure varies among individuals.